A Prescription for Problems: The Dangers of Antibiotics
We are at the end of another cold and flu season, were you one of the millions of Australians that took antibiotics?
According to the National Prescribing Service (NPS), Australians are addicted to using antibiotics for every sniffle and cough, and are among the highest users of antibiotics in the world.
The organisation cites figures from 2006 when 22 million prescriptions were dispensed by community pharmacies, and estimates that at least three million of these were wasted on viral infections.
Today, some strains of bacteria that cause infections have become so resistant to many antibiotics that people are again dying of infections.
In Australia, antibiotic-resistant bacteria are thought to cause more than 7000 deaths each year.
Antibiotics of all kinds are now the go-to prescription for just about every illness. At this point, our reliance on them is more like abuse. Antibiotics are used all too commonly – for diseases they can’t even treat—and that’s resulting in their overall ineffectiveness.
Not only does such frequent pill popping cause relatively unknown side effects, but it can become deadly on a global level if it continues unabated.
Antibiotics have prevented countless deaths since their creation, but even too much of a good thing can have disastrous results. The worst part is that most people, including some in the medical industry, aren’t fully aware of the problem.
In March 2009, pharmacies around the U.S. gave away free antibiotics to promote health in cash-strapped times.
Luckily, the Centers for Disease Control and Prevention (CDC) stepped in and advised people against treating antibiotics like all-purpose medicine or, even worse, taking them like multivitamins.
Therein lies the biggest problem with antibiotics overuse—people think of them as wonder drugs that can heal anything. But they’re effective only against bacteria, so if someone has an ear infection, tuberculosis, or other bacterial infection, an antibiotic prescription makes sense.
Antibiotics don’t have any effect on viral illnesses, including colds and flus.
Unfortunately, this fact has been lost in a sea of misinformation. A survey that Food borne Diseases Active Surveillance Network conducted from 1998 to 1999 found that 32 percent of the population believed antibiotics should be taken for colds.
Over half of those surveyed were unaware of any potential risks associated with them. But consumers aren’t the only ones perpetuating the myth—in 2001, over 31 percent of antibiotic prescriptions were for colds or sore throats.
When Medicine Gets Deadly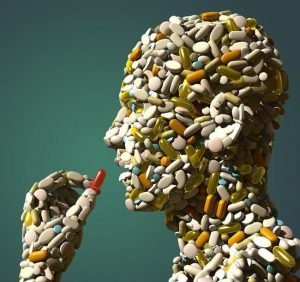
Even if the really serious side effects are isolated to small parts of the population, antibiotics’ increasing ineffectiveness is a problem that impacts all of us.
Antibiotics work by flushing out all bacteria—including the good kind that keeps us healthy, which is another big problem—out of our systems to get rid of the infection.
But when they don’t eradicate all of the bad kind, it results in hyper-resistant bacteria that require a stronger form of antibiotics.
Doctors in hospitals and clinics around the world are losing the battle against an onslaught of new drug-resistant bacterial infections including staph, pneumonia, strep, tuberculosis, dysentery and other diseases that are costly and difficult, if not impossible, to treat.
These superbugs leave scientists scrambling to create new and more potent treatments, but the overuse of antibiotics leaves them with very little to work with anymore. Now there are a multitude of bacterial strains that no existing antibiotic can treat.
Immune Suppression
This may sound odd, as the purpose of antibiotics is presumably to help the immune response. However, evidence indicates that people treated with antibiotics have more repeat infections than those who are not treated.
In fact, antibiotics do not aid the immune system, they replace one of its functions.
Antibiotics act by inhibiting certain enzymatic processes of bacteria, and by changing mineral balances. Normal cells, however, are also affected. This may be one reason why antibiotics weaken the immune response.
Overgrowth of Candida And Other More Dangerous Intestinal Infections
Normally, candida albicans, a common yeast, lives peacefully in our intestines and elsewhere, in harmony with other flora that keep the yeast in check. Take an antibiotic and all of this changes.
By suppressing the normal flora, candida takes over and problems begin. In its mild form the result is diarrhoea or a yeast infection. Far more serious is the growing problem of chronic muco-cutaneous yeast infection.
One of the prime risk factors for chronic candida infection is repeated antibiotic use.
Even more dangerous is that antibiotic use opens the intestines to infection by other species of pathogenic or disease-causing bugs, parasites, yeasts and other types of organisms ranging from amoebas to far more toxic ones that can cause all types of systemic damage, as well as damage to the intestinal lining and related areas.
Antibiotics and Cancer Link
A 2008 study of 3,000,000 people divided the participants into groups that had taken no antibiotics for the past two years, those that had taken 2-5 prescriptions and those that had taken six or more prescriptions in the same time period.
Participants were tracked for six years afterwards. Those who had taken 2-5 antibiotic prescriptions had a 27% increase in cancers compared to those who took none. Those who took six or more prescriptions had a 37% increase in cancers.
Antibiotics Kill All Bacteria in the Body – Including the Ones We Need
Like pesticides, antibiotics kill good bugs along with the bad ones. Broad-spectrum antibiotics are notorious for this.
The human intestine has a somewhat delicate ecology in which certain bugs help digest food, produce certain vitamins, and maintain a balance of organisms that prevents harmful bacteria and yeasts from multiplying.
The impact of antibiotics on the normal gut flora has previously been thought to be short-term, with any disturbances being restored several weeks after treatment. However, a recent review into the long-term impacts of antibiotic therapy reveals that this is not always the case.
Studies have shown that high levels of resistance genes can be detected in gut microbes after just 7 days of antibiotic treatment and that these genes remain present for up to two years even if the individual has taken no further antibiotics.
Of equal concern is the impact of antibiotic warfare on our gut defense systems. The casualties of antibiotic therapy include our beneficial bacteria as well as the lining of the gut.
While damaging bacteria are being eradicated, they can also promote damage to the mucosa effectively making it “leaky”. This significantly impacts upon how well we absorb nutrients as well as how well we cope with invaders.
Labelled “Leaky Gut Syndrome”, a side effect of antibiotic therapy is gut inflammation and irritation. The end result is metabolic and microbial toxins of the small intestines to flood into the blood stream.
This event compromises the liver, the lymphatic system, and the immune response including the endocrine system.
 Resistant Strains in Hospitals
Resistant Strains in Hospitals
Clostridium difficile, or C. difficile is an organism on the rise. Once confined mostly to hospitals and other health care facilities, C. difficile is extremely prevalent and the strain is deadlier than ever.
It’s actually brought on in part by antibiotic use—the drugs kill off the beneficial bacteria in our guts, making way for C. difficile to take root.
Even after treatment—which is another round of antibiotics—some patients continue showing symptoms.
An estimated 20 percent of affected people will get sick all over again later.
Emeds Comment
Antibiotics are an interesting class of medications that can save lives. However, antibiotics are overprescribed and toxic. They should be used as a last resort, not the first.
Very often, simple, inexpensive natural methods described here work better with far fewer adverse effects.
This doesn’t mean that antibiotics don’t have their place in medicine; in some cases, their improvement to our well-being has been immeasurable.
But in order to keep it that way, we need to understand and respect their limits.
As the old saying goes, everything in moderation–even when it’s something as helpful as medicine.
Probiotics
Unlike antibiotics, which means “to destroy life,” probiotics literally means “life giving.”
If you have taken a course of antibiotics recently probiotics are your first line of defence – this is what you can do to help your immune system build back up.
By re-populating your digestive system with probiotics you can effectively treat conditions like diarrhoea, candida overgrowth, eczema and skin conditions, Crohns Disease and Inflammatory Bowel Disease (IBD) to name a few.
If you have to take a course of antibiotics, taking a probiotic at the same time will lessen the adverse effects that they will have on the good bacteria in your gut. Continuing on probiotics after the course of antibiotic therapy will also promote a healthy gut microflora.
This can often prevent acute dysbiotic conditions like Candida Overgrowth (thrush).
The fastest way to re-populate your good bacteria is by taking a 7 day dose of Bioceuticals UltraBiotic 500. This high strength 14 strain probiotic supplement contains 500 billion bacteria per sachet.
Click here for Emeds Best Probiotics.
Glutamine
When you take a course of antibiotics the intestinal mucosa is injured and little holes can appear – this is called Leaky Gut. Bacteria penetrates the intestinal wall and enters adjacent tissue, and can enter the bloodstream.
Glutamine, an amino acid, is essential to repair the gut lining.
Glutamine is not only beneficial for chronic antibiotic misuse but can help any kind of inflammatory bowel disease including Crohns, IBD and food allergies.
Anti Inflammatory Mucosal Support provides Glutamine, Aloe Vera and zinc to restore intestinal gut lining.
Iodine – Antibiotic, Antiviral and Antiseptic
Iodine offers a serious and potent replacement for much of the antibiotics and can be used safely with children.
Though it kills 90 percent of bacteria on the skin within 90 seconds, its use as an antibiotic has been ignored. Iodine exhibits activity against gram-positive and gram-negative bacteria, molds, yeasts, protozoa, and many viruses.
Iodine kills single celled organisms by combining with the amino acids tyrosine or histidine when they are exposed to the extra-cellular environment.
All single cells showing tyrosine on their outer cell membranes are killed instantly by a simple chemical reaction with iodine that denatures proteins.
Nature and evolution have given us an important mechanism to control pathogenic life forms and we should use it and trust it to protect us in ways that antibiotics can’t.
Bioceuticals Iodine Drops provide an easy to dose supplement that can be taken internally.
To find out more about Iodine click here.
Garlic
Garlic is a powerful, natural antibiotic – and it doesn’t kill off our healthy bacteria like prescription antibiotics do.
Unlike chemical antibiotics, garlic is also an effective antiviral and antifungal – and taking just a few cloves of garlic each day can really speed infections away.
The antibacterial property belongs to the garlic constituent allicin, which is released when you cut a garlic clove. This activate phagocytes, B-Cells, and T-cells — all three levels of the cellular immune system.
For those of you that can’t handle eating raw garlic then Garlic Forte is a great product for natural treatment of colds and flus.
It also contains immune boosting and anti-viral herbs like Echinacea, Andrographis and Astragalus.
Vitamin D
It’s a beautiful thing that vitamin D is one of the most important vitamins there is and that it’s free! Get outside and get some sun. Some sun without sunblock!
Vitamin D plays a crucial role in triggering and arming immune cells like T-Helper cells.
For T cells to detect and kill foreign pathogens such as clumps of bacteria or viruses, the cells must first be ‘triggered’ into action and “transform” from inactive and harmless immune cells into killer cells that are primed to seek out and destroy all traces of invaders.
Food sources of vitamin D can’t even come close to the amount of vitamin D your skin produces.
And since we’re told to avoid the sun because it’s going to kill us, most of us are vitamin D deficient.
Click here for Emeds Best Vitamin D supplements.
Relax!
Constant stress is an immune system killer. With our daily hustle and bustle, most of us don’t get a chance to catch our breath.
We keep our cortisol levels sky-high with work stress, family stress, the stress of the commute, hurried lunches, and late nights.
So turn off the news, which tends to do nothing more than stress people out, and take up a hobby. And being outside in a natural setting, perhaps hiking or just hanging out at the park allows you to relax and get some sun.
Final Word
Always ask questions – If a doctor prescribes you an antibiotic, ask them what effect antibiotics will have on your condition and if they are really necessary.
If these questions annoy your doctor, then get another doctor. You have a right to know what you are taking and why.
Further Reading:






